What is Fibromyalgia
Fibromyalgia, also known as Fibromyalgia Syndrome (FMS), is a debilitating, chronic disease characterized by body aches, fatigue, and pain in specific points in the body. Insomnia, lack of concentration and mood disturbances may also accompany these symptoms. In recent years more is being understood about the disease and its causes and diagnosis.
According to the medical dictionary: fibromyalgia is a neurosensory disorder characterized by widespread muscle pain, joint stiffness, and fatigue. The condition is chronic (ongoing), but pain comes and goes and moves about the body. The disorder is often misdiagnosed or unrecognized and is and often complicated by mood and anxiety disorders.
Fibromyalgia syndrome is also subject of keen psychiatric interest. Dr. Bradley* explained that fibromyalgia may be part of a group of affective spectrum disorders (ASD). The ASD hypothesis proposed by Hudson† and colleagues suggests that this group includes, but is not limited to, 10 psychiatric and 4 medical disorders that share 1 or more physiologic abnormalities important to their aetiology. These include inherited factors that may contribute to enhanced pain sensitivity, diminished pain inhibitory function, or mood disorders. Studies of patients, as well as their first-degree relatives, with fibromyalgia or rheumatoid arthritis have provided evidence to support the ASD hypothesis. For example, Arnold** and colleagues reported that the first-degree relatives of patients with fibromyalgia, compared with those of patients with rheumatoid arthritis, more frequently met diagnostic criteria for fibromyalgia or major depressive disorder (MDD) and exhibited a greater number of sensitive tender points (i.e., enhanced pain sensitivity). Hudson† and colleagues further examined data from this family study and found that fibromyalgia co-aggregated with 1 or more other forms of ASD whether mood disorders were included (p = .004) or not (p = .012). These findings suggest that, consistent with the ASD hypothesis, (1) heritable as well as environmental factors may contribute to family aggregation of pain sensitivity in fibromyalgia, (2) fibromyalgia co-aggregates with other affective spectrum disorders, and (3) these disorders may share heritable physiologic abnormalities.
** Lesley M. Arnold, Ph.D., University of Cincinnati College of Medicine, Cincinnati, Ohio 45267-0559, USA. Lesley.Arnold@uc.edu
†James I. Hudson, MD, ScD, SM, Biological Psychiatry Laboratory, McLean Hospital Department of Psychiatry, Harvard Medical School, Belmont, MA 02478, USA. jhudson@mclean.harvard.edu
Fibromyalgia 1990 – 2010
American College of Rheumatology had appointed a group medical doctors that formed Multicenter Criteria Committee who defined criteria for the classification of fibromyalgia in 1990. This has been presented in the bookmark → diagnosis .
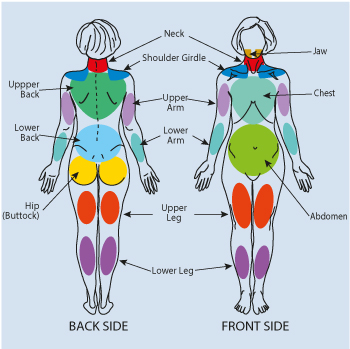
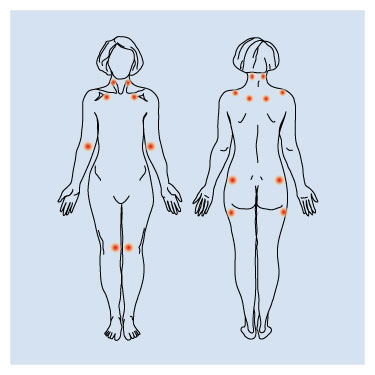 Fibromyalgia belongs to the group of illnesses defined as "soft tissue rheumatism" or "non joint rheumatism". The illness belongs to the most common peri-articular* chronic pain non-inflammatory disorder. The widespread pain is accompanied by hyperaesthesia in characteristic localization – so called tender points. Moreover, heavy, general, and chronic tiredness (chronic fatigue syndrome), sleep disturbances, and low mood or depression often occur. All these symptoms defined as the major criteria are accompanied by other various and more or less intense symptoms and disorders called as vegetative or functional.
Fibromyalgia belongs to the group of illnesses defined as "soft tissue rheumatism" or "non joint rheumatism". The illness belongs to the most common peri-articular* chronic pain non-inflammatory disorder. The widespread pain is accompanied by hyperaesthesia in characteristic localization – so called tender points. Moreover, heavy, general, and chronic tiredness (chronic fatigue syndrome), sleep disturbances, and low mood or depression often occur. All these symptoms defined as the major criteria are accompanied by other various and more or less intense symptoms and disorders called as vegetative or functional.
It is estimated that, even in the US where fibromyalgia awareness is relatively high, it takes approximately five years from first symptoms to the final diagnosis. Patient sees at least 15 doctors of various specialities in that time. The variety and number of symptoms accompanying fibromyalgia is a real nightmare for patients and causes frequent and unproductive visits to different specialists and various examinations like blood tests as well as imaging scans (x-rays, NMR**, CT scans†, and USG scans‡.
**NMR - nucelear magnetic resonance or magnetic resonance imaging is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body in both health and disease.
†CT - computed tomography scan is imaging technique that can reveal anatomic details of various internal organs and structures that cannot be seen in conventional X-rays.
‡USG - medical ultrasound (also known as diagnostic sonography or ultrasonography) is a diagnostic imaging technique based on the application of ultrasound. It is used to see internal body structures such as tendons, muscles, joints, blood vessels, and internal organs. Its aim is often to find a source of a disease or to exclude any pathology. The practice of examining pregnant women using ultrasound is called obstetric ultrasound, and is widely used.
Fibromyalgia after 2010
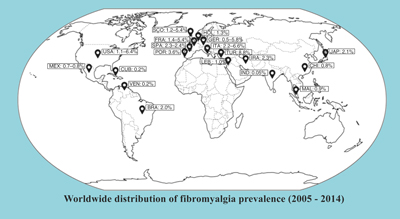
It is important to understand the impact of this illness on patient, her/his family, and community, when investigating fibromyalgia epidemiology. The modified new ACR diagnostic criteria of fibromyalgia in 2010 enables to perform broad epidemic research in different countries and continents without a necessity to examine tender points. This also would make possible to evaluate socio-demographic determinants of fibromyalgia and its coexistence with other disorders.
On the base of many (several dozen) epidemic survey performed according to fibromyalgia diagnostic criteria published by ACR in 1990 the average rate of fibromyalgia prevalence was 2.7 % of the total world population.
There are available three surveys applying the new (2010) diagnostic criteria of fibromyalgia, only (in the USA1, Germany2, Tailand3). It seems that the new criteria are more sensitive and less specific as compared to the old (1990) ACR diagnostic criteria. This may reflect on increased number of diagnosed fibromyalgia cases.
2 Wolfe F, Brähler E, Hinz A, Häuser W. Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res. 2013;65:777–85. A large, nationwide epidemiological study of FM in Germany, using the 2010 ACR diagnostic criteria for FM.
3 Prateepavanich P, Petcharapiruch S, Leartsakulpanitch J. Estimating the prevalence of fibromyalgia and its impacts on health in thais: a community-survey in Bangkok, Thailand [Abstract]. Value in Health. 2012;15:A678.